The Safe Laser 1800 Vs. 500: 10 Major Differences Between Wavelength And Power Output
The photobiomodulation (PBM) devices, like the Safe Laser 1800 & 500, are fundamentally controlled by the technical parameters they use. Wavelength and power output are two of the most important. Although both devices work on the same fundamental principles of science, their specific variations in these parameters determine their unique application in clinical practice, their treatment efficacy as well as the degree of treatment. The wavelength is the determining factor for the placement of the light energy within the body. The power output determines the amount and speed of energy that is delivered. A thorough analysis of these variables reveals the reason the Safe Laser 1800 is engineered as a powerful deep tissue unit that is suitable for high-volume clinics and the Safe Laser 500 is designed to be a multi-functional, portable device for both superficial and mid-depth therapy.
1. Primary Wavelength: A shared basis to allow deep tissue penetration
Safe Laser 1800 & Safe Laser 500 both utilize the infrared wavelength 810 nanometers (nm) as their principal source. This is a deliberate and scientifically-grounded choice. The wavelength (810 nm) is within the therapeutic range (650-950nm) where the penetration of light into skin, blood and water is maximized. This particular wavelength triggers photobiomodulation by optimally absorbing cytochrome c in mitochondria. Thus, the fundamental mechanism that reduces inflammation and pain, as well as promoting healing in deep tissues (muscles joints, ligaments, and joints) is the same and consistent for both devices.
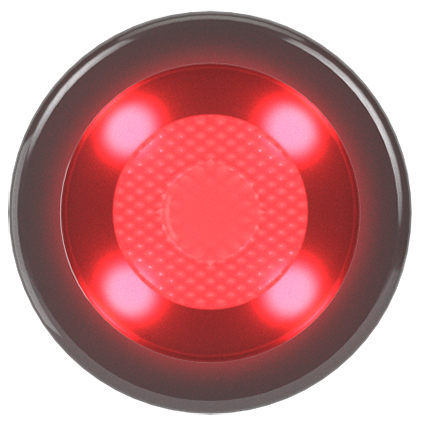
2. The Safe Laser 500 Hybrid Wavelength Systems 810 nm and 660 num
One of the main distinguishing features of the Safe Laser 500 is its application of a hybrid "cluster" application. The central diode emits 810nm light, it is also surrounded by rings of SuperLuminous Diodes which emit 660nm light. This wavelength of red light is more easily absorbed by hemoglobin as well as other superficial chromophores. The wavelength of 660 nm is highly efficient in treating superficial ailments like acne, open wounds as well as skin ulcers. The 500 offers the dual wavelength therapy that is simultaneously targeting deep (with 810nm nm wavelength) and superficial (with the wavelength of 660nm) tissues.
3. The Secure Laser 1900's 810nm focal is a single, high-power laser.
Safe Laser 1800 is a laser with a single 810nm diode. It is more powerful. It does not have any additional waves. The design philosophy of the Safe Laser 1800 is to focus intensity with maximum penetration depth. Through concentrating its immense power in a single 810nm wavelength that penetrates deeply, it can block absorption or scattering which happens when tissues are or dense. It is therefore the best instrument to penetrate deep joint capsules and spine of those with greater body weight.
4. Peak Power Output A Quantity Differential
The biggest difference is in the power at peak. The Safe Laser 1800 produces a peak power of 18 Watts (or 18,000 milliwatts). Safe Laser 500 has a maximum output of 5 Watts (5, 000 milliwatts). This means the SL 1800 has more than 3.5 times the raw power of the SL 500. The differences in power are not due to efficacy. It's about efficiency and the capability of delivering a significant therapeutic dose for difficult, deeply-rooted diseases.
5. Treatment times, and efficiency of clinical care
The power output is the determining factor for the duration of treatment. The dose of therapeutic treatment in PBM is determined in Joules (Energy = Power x Time). For 100 Joule dose for the Safe Laser 1800, at 18W, will take approximately 5.5 minutes. Safe Laser 500 at 5W will take about 20 seconds to give 100 Joules. If a treatment plan requires 500 Joules it would be approximately 28 seconds instead of 100 seconds. In busy settings, these time savings are transformational. They permit faster patient rotation and the treatment of larger areas.
6. Beam Divergence And Treatment Areas The Coverage
The type of light that is emitted differs. Safe Laser 1800 uses divergent laser beams from its single large-diameter nozzle. The beam expands as it leaves the applicator. Covering a larger area (several cm in size) of skin. This is the best treatment for large areas of discomfort or inflammation, like quadriceps or a strained lat. Safe Laser 500 has a cluster head that is focused on an application point. This makes it better at targeting localized structures such as triggers or tendon. The 660-nm circular area targets the tissue immediately surrounding the area.
7. Coherence in Photon Behavior
Safe Lasers 1800 source at 810 nm has a true coherent wavelength. Coherent light, in which photons are in phase, is thought to penetrate tissues more efficiently due to less scattering, a phenomenon called "superradiance." This may contribute to its greater depth penetration. The Safe Laser 500's central diode (810 nm) is also coherent, while the surrounding 660nm SLDs (though they are still monochromatic) aren't coherent. Non-coherent light scatters more readily which can be beneficial for treating superficial wounds as it gives a more uniform, diffuse coverage over the surface area.
8. Wavelength and Power dictates clinical indications
The differences in their design define their best applications in clinical practice. Safe Laser 1800 is a high-powered laser having only a single wavelength of 810nm. It is ideal to treat deep joint pathologies like hip osteoarthritis, spinal facet syndrome, as well as deep muscle strains and chronic, inflamed joints. Safe Laser 500 excels in treating acute soft-tissue conditions (sprains and tendinitis), as well as wound care, surgical scars, and post-operative scars.
9. Dosimetry – Practical Application
The power difference affects the way a practitioner thinks about dosing. The time of exposure per spot is the most important variable in the Safe Laser 1800. It is extremely brief. The practitioner must be diligent to maneuver the device properly so as to not over-treat one spot because of the fast energy delivery. The longer treatment times are forgiving when using the Safe Laser 500 and align perfectly (on specific models) using the automated dosage guides, which determine the duration of treatment depending on the chosen condition and power settings.
10. Strategic Summary Power vs. Versatility
It is important to make a decision based on the power and wavelength. Safe Laser 1800 sacrifices the multi-wavelength flexibility and speed of the 500 in order to reach unparalleled depth. It's a powerful clinical tool designed for the most demanding of conditions. The Safe Laser 500 is a tool of versatility and portability, offering a combined-wavelength approach in a compact format, making it ideal for mobile therapists or those focusing on a wider variety of superficial-to-mid-depth conditions. Both devices are extremely powerful, but each is designed to work in a distinct therapy field. See the recommended bemer ágy for website info including lézeres kezelés sarkantyúra, lézerterápia árak, safe laser tapasztalatok, infravörös lézer, safe laser készülék, safelaser hu, lágy lézer otthonra, széf lézer, lezer terapia, soft laser árak and more.
Top 10 Tips For Tracking The Progress And Results With Safe Laser Devices
It is essential to keep track of progress and outcomes, but this is often overlooked. This is the primary element to success with PBM therapy using Safe Laser devices. Without objective and subjective evidence it is impossible to assess effectiveness, adjust treatment parameter or justify the need for continued care to insurance companies or patients. Effective tracking turns anecdotal observations into a structured, scientifically based practice. This multi-faceted approach records quantitative data as well as the feedback of patients in a qualitative way beginning with the initial baseline evaluation and concluding with the final outcome. This approach does more than help in the making of clinical decisions, but it also empowers and enables patients to track their progress, which can improve adherence.
1. Setting up the Comprehensive Baseline Assessment
Before the initial treatment, it is important that a baseline be completely established. This will serve as the benchmark to which the progress of the treatment will be measured. A robust base includes:
Subjective Pain Scales Using a standardized Numeric Pain Rating Scale (NPRS) or Visual Analog Scale (VAS) to track pain intensity during moving, at rest, as well as at night.
Functional Assessment: Documenting specific functional limitations (e.g., "unable to lift arm above shoulder level," "can only walk 10 minutes").
Objective Measures can be described as goniometry, strength measurement, circumferential measurements of swelling and Dynamometry.
Quality of Life Indicators Note impact on sleep, mood and ability to perform daily Activities (ADLs).
2. The importance of a standardized treatment log
A meticulous treatment journal is essential to keep track of. The following details should be recorded for every treatment session:
Date and time for treatment
The Anatomical Sites and Conditions treated (e.g. medial left knee femoral cuneyle; the proximal attachment of right supraspinatus).
Treatment Parameters : Total energy that is delivered to every site (in Joules) and the power setting, and the duration of treatment in total.
Patients' Immediate response any feedback received during or immediately after the session.
3. Instruments for Validated Outcomes Measurement
To guarantee objectivity and permit comparison, practitioners should employ validated outcome tools. Common tools for musculoskeletal disorders include:
The Oswestry Disability Index is a measure of lower back pain.
The Shoulder Pain and Disability Index (SPADI).
The Lower Extremity Functional Scale for Hip/Knee Arthritis (LEFS or HOOS/KOOS).
These tests can give a quantifiable result that can be tracked over the course of time. It offers a clearer view of functional improvement rather than pain scores.
4. Re-Assessment Periodically, at Defined Time Intervals
The progress should not be estimated; it should instead be monitored regularly and at pre-determined intervals. A standard procedure is to revisit the most important metrics (pain scales and primary functional limitation ROM) after every 3-5 sessions of treatment. The practitioner can determine whether the treatment is effective or if there are some parameters that need to be changed by checking in frequently. Weekly or biweekly re-evaluations with full scores on outcome tools, may be more comprehensive.
5. Documenting the "Healing Crisis" and Interim Variations
Tracking should take into consideration the changes during the process of healing. Users have noted that some patients might experience symptoms that are temporary getting worse, also known as "healing crises," following the initial treatment. It is crucial to record this. This will allow you to differentiate between a healing reaction and an adverse reaction or an ineffective treatment protocol. It is important to note that the patient's discomfort went from a 4/10 rating to a 6/10 rating after two days, but then fell to 3/10 after four days. This gives important information and can help avoid prematurely discontinuing an effective treatment.
6. Documentation in photographic form
Serial photography provides a useful monitoring tool for conditions that are visible, like wounds, skin lesions, edema and bruises. The identical angle, distance and lighting should be used for each assessment point. This will show evidence of improvement, for example shrinking of swelling, or the fading of bruising, or wound contraction.
7. Logs and diaries created by patients
The ability to keep track of their progress over time increases engagement as well as providing data from real life. A simple diary allows patients to keep track of their daily pain level along with the medication they are taking and any other activities they complete. The data can help identify patterns that aren't evident in a clinical setting, such as the discomfort that is associated with certain movements, or a change in the quality of sleep.
8. Monitoring dosages and parameter adjustments
PBM is dose-dependent. The treatment journal must document all changes made to treatment regimen. The treatment log should be logged along with the patient's progress. This creates a feedback loop that allows the practitioner to know what parameters and treatments are most effective.
9. Long-Term follow-up for Chronic Conditions
For chronic illnesses, the tracking should not end when active treatment ends. After the final treatment is completed, scheduling a one month and three-month follow-up can provide important details about long-term outcomes. This lets you distinguish between pain relief for a short time and longer-lasting tissue repair and reconstruction. This test can also help find patients who might be benefited from a "booster treatment" frequently to help maintain the gains.
10. Data Analysis and Interpretation the process of making clinical decisions
The final and most important stage is synthesis of all of the data collected to make educated decisions. Tracking is useless without interpretation. Does the patient's score on pain decreasing over time? Are there improvements in their functional score? Are they seeing any improvement in their ROM? If the answer is yes, the procedure which is being utilized is effective and should be kept in place. The data will show whether the progress has slowed down or reversed. If it is the case you should alter the method, possibly by adjusting the dose, targeting other structures or looking at other factors. Safe Laser therapy is delivered efficiently and effectively for each patient by this data driven cycle. Take a look at the best baker ciszta otthoni kezelése for more advice including soft laser terápia, safe laser 500 bérlés, orr lézer készülék, soft lézer kezelés ára, safe laser kölcsönzés, lágylézeres készülék, safe laser kölcsönzés, bemer nyíregyháza, safe laser vélemények, lézeres kezelés sarkantyúra and more.

